Labral Injuries
What is the glenoid labrum?
The glenoid is the cup of the shoulder joint, and the labrum is a rim a cartilage at the edge of the glenoid. The labrum functions as a seal to the shoulder joint, and also helps with stability of the shoulder. The labrum itself serves to deepen the glenoid, to provide more surface for the humeral head (ball) to articulate with. More importantly, the glenoid labrum serves as the attachment of several ligaments that ensure the stability of the normal shoulder joint.
What problems can occur with the labrum?
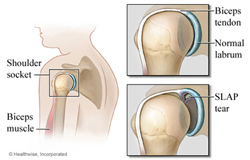 The labrum can have several sorts of problems, from traumatic tears and degenerative tears, multi-directional instability, micro-instability and internal impingement. One of the more commonly known problems is tearing of the glenoid labrum. This can occur in two ways. First, in younger patients, a traumatic tear can happen with a sudden force placed on the labrum (shoulder dislocation, "jamming" the shoulder). Patients can usually recall a specific incident or injury that was the likely cause.
The labrum can have several sorts of problems, from traumatic tears and degenerative tears, multi-directional instability, micro-instability and internal impingement. One of the more commonly known problems is tearing of the glenoid labrum. This can occur in two ways. First, in younger patients, a traumatic tear can happen with a sudden force placed on the labrum (shoulder dislocation, "jamming" the shoulder). Patients can usually recall a specific incident or injury that was the likely cause.
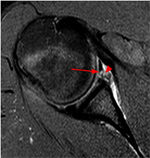
In the case of a suspected traumatic tear, we will obtain plain xrays to evaluate the bony structure of the glenoid and the humeral head. Following this, we will most often refer the patient for advanced imaging, i.e., a MRI. Oftentimes, labral injuries are difficult to see with a standard MRI. Because of this, injecting dye into the shoulder joint immediately prior to the MRI will help show the anatomy of the joint better. This is called an MRI-arthrogram.
 A degenerative tear is similar, but the mechanism is usually due to repetitive strains placed on the labrum over time. In patients who have glenohumeral arthritis, we often see degenerative labral tears.
A degenerative tear is similar, but the mechanism is usually due to repetitive strains placed on the labrum over time. In patients who have glenohumeral arthritis, we often see degenerative labral tears.
Multi-directional instability is caused by a generalized laxity (looseness) of the supporting ligaments attached to the glenoid labrum. Usually, there is no labral tearing, but in some cases, the labrum can be torn in one or more places. This is more common in younger patients, who are often swimmers or who play overhead sports such as raquet sports, and throwers.
Micro instability and internal impingement are closely related. In fact, both are part of a process that can eventually lead to a labral tear. This process is common in throwing athletes such as baseball pitchers, fielders, and quarterbacks. It most often starts as shoulder tightness, which leads to loss of motion. This loss of motion is caused by the shoulder joint capsule tightening up. With the capsule tightening, this can cause the posterior superior labrum to become pinched between the bony glenoid and the humeral head when the shoulder is elevated. This is called internal impingement. When internal impingement is not treated, it can lead to micro instability, which is a very small tear in the posterior superior labrum, which is often so small that it may not be seen on an MRI arthrogram. If this is not treated, it can lead to a frank labral tear.
What are the symptoms of a labral injury?
Most patients report shoulder pain, especially with overhead activities, or with reaching across the body. There is sometime a feeling of instability, as if the shoulder "slips around," doesn't feel right, subluxates (nearly dislocates), or even frankly dislocates. Some patients also report weakness, again with overhead activities, and with reaching across the body. However, as noted, the main complaint is usually that of pain.
What are the treatments for labral injuries?
The treatments for labral injuries are similar to those for other shoulder disorders. Initially, we will recommend a course of relative rest, possibly of non-steroidal anti-inflammatories, and avoidance of aggravating activities. However, most patients with labral tears are very active and don't want to give up their activities, so we often progress more rapidly to physical therapy. In the case of labral injuries, especially early on with internal impingement, micro instability, and multidirectional instability, the physical therapy regimen focuses more on capsular stretching and scapular stabilization (regaining the normal mechanics of the shoulder joint). There is less focus on strengthening until therapy has been ongoing for at least several weeks.
Is surgical treatment necessary for labral injuries?
In some patients, a course of aggressive non-operative treatment is not successful in treating their symptoms and helping them regain the quality of life they desire. When this happens we will typically recommend surgical intervention. A labral repair can either be done in an open fashion, or arthroscopically. Dr. Hergan prefers to use the arthroscope for its advantage in attaining an anatomic repair with less trauma to the tissues surrounding the shoulder joint.
If a patient elects to have surgery an arthroscopic technique is utilized. The arthroscope (camera) is introduced into the shoulder joint and a systematic examination of all the structures of the shoulder joint is performed. Visualization of the ligaments, the rotator cuff, biceps tendon, and the articular cartilage is all possible. We then focus on the labrum. The labral injury is identified, the glenoid bone is prepared, and the labrum is then secured anatomically to the bone using small anchors with attached suture (similar to those used in rotator cuff repairs).
What is the post-operative course?
Following surgery, patients are placed into a sling and advised to do no more than passive pendulum exercises (allowing the arm to dangle in front of the body while leaning forward). Labral surgery is a day surgery, and patients are discharged home in the sling and with pain medications.
We have patients return to the office approximately seven to ten days after surgery for wound checks, suture removal and for a prescription to start physical therapy.
Postoperatively, the therapy program is focused on passive motion until six weeks after surgery, allowing the labral tissue to heal. Active assisted motion is then started and progressed to active motion over the next three to four weeks, allowing the repair to mature. No strengthening activities are allowed for three months.
If all goes as anticipated, the total healing time is between three and four months. However, for athletes, return to sport is not allowed for six months after surgery. At the six month point, a throwing program is initiated, patients are allowed to start lifting weights in moderate amounts, and other athletic activities are added under the direction of a licensed trainer or physical therapist.
Our goal at Middlesex Orthopedic Surgeons is to provide high quality care, both non-surgical and surgical, that eventually will allow patients to regain lost function and experience pain relief that will then result in the improvement of their quality of life. Through state of the art care, our aim is to facilitate a return to pre- injury level of function that will ultimately be satisfactory to our patients.
Dr. David Hergan is a labral tear surgeon who specializes in the treatment of labral injuries in the Connecticut area. For all appointments and inquiries, please call (860) 669-4197 (860) 669-4197 or click here to request an online appointment.