Shoulder Resurfacing
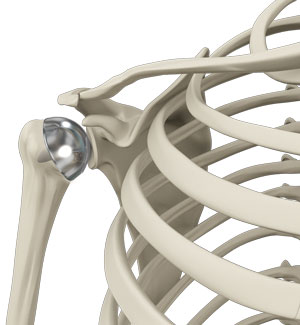
Shoulder arthritis is an inflammatory condition causing pain and stiffness in the joint. It can be successfully treated with total joint replacement surgery which is commonly performed on older patients. However, the surgery is not advisable for young active individuals due to concerns with durability of the implants used in replacement surgery. Joint replacement surgery uses metal and plastic prostheses to replace the damaged cartilage of the shoulder joint. Extensive activity in young individuals can cause loosening or failure of the prosthesis, requiring revision surgery.
Biological resurfacing is a procedure to resurface the degenerated or arthritic articular surfaces of your shoulder joint with an allograft (biological graft).
Disease Overview
The shoulder joint is a ball and socket joint formed by the humerus (upper arm bone) and the glenoid socket (a cup like depression on the shoulder blade). The articular surfaces of the joint are lined by smooth cartilage that may undergo degeneration or damage as a result of infection, trauma, overuse, prior surgery, osteoarthritis or avascular necrosis. This can lead to pain and loss of motion adversely affecting your daily activities.
Indications
Biological shoulder joint resurfacing is indicated in young, active individuals under 50 years old with a relatively flexible arthritic shoulder joint with large areas of defects that have not been successfully treated with conservative methods such as pain medication, physical therapy or corticosteroid injections.
Surgical procedure
The shoulder joint preservation procedure is performed under general anesthesia on an outpatient basis with the patient in a semi reclined or beach chair position.
The surgery is performed as a minimally invasive arthroscopic procedure. Two small incisions are made – one above and the other below your shoulder.
An arthroscope, a narrow tube with a camera and light on the end, and tiny surgical instruments are introduced through these incisions. The arthroscope provides your surgeon with a clear view of the surgical site. The diseased tissue is removed (debrided), and the humeral and glenoid defects are identified.
A guide pin is drilled through the humeral head creating a tunnel that reaches the defects in the articular surface of the humeral head.
The tunnel is used to guide instruments to drill and prepare both the humeral head and glenoid articular surface defects.
Healthy osteochondral grafts consisting of cartilage and subchondral bone are removed from the humeral head, medial tibial condyle (part of the knee) or distal tibial plafond (close to the ankle) of a deceased donor. The allograft is then prepared and size-matched to fit the defects. A hole is made in the center of the humeral graft and a suture inserted to help in positioning the graft into the humeral defect. The allograft is then introduced into the humeral defect and press fit into place. The procedure is repeated for the glenoid defect and the allograft is held in place by chondral darts. Using the arthroscope, the surgeon ensures the allografts are accurately positioned. The arthroscope and instruments are then removed and the incisions closed.
Post-Operative Care
Following surgery, you are placed in a sling for a week after which you will begin passive assisted range of motion exercises. Active range of motion exercises begins 2 weeks postoperatively and is followed by strengthening exercises at 6 weeks post op.
Advantages & Disadvantages
Biological resurfacing is advantageous as it:
- Avoids implant failure of a total shoulder replacement which is higher in young active individuals
- Has a quick recovery period
- Less trauma and decreased post op pain
- Reduced risk of infection
- Use of natural bone grafts instead of artificial prostheses helps achieve normal anatomical structure and function to the joint
- Rotator cuff and large shoulder muscles are not cut or damaged
Disadvantages include:
- Long term failure
- Eventually requires replacement surgery
Risks and complications
As with any surgery there are risks involved. Complications that can occur following biological shoulder resurfacing includes:
- Bleeding
- Infection
- Blood clots
- Graft failure
- Shoulder stiffness or weakness
- Persistent pain
- Damage to adjacent nerves or blood vessels